
“How long will it be before you know if the immunotherapy is working?”
“Why are we taking family photos?”
“Have they told you what stage his metastatic melanoma is?”
“How are YOU doing?”
“What is your treatment team’s success rate?”
“How can we help?”
“Is most of the hardship with your husband’s illness?”
“Has someone talked to you about alkaline water, non-hallucinatory cannabis oil, eliminating sugars, eliminating GMOs, essential oils, or Protandim supplements?”

When you’re ill or caring for someone who’s seriously ill, you get asked a LOT of questions. I can tell you with 100% certainty that most of the questions aren’t nearly as easy to answer as you’d think. And as far as the questions you ask yourself? There are way more questions than answers.
The doctors can’t say for sure when they’ll know if immunotherapy is working. Maybe 12 weeks, maybe 24 weeks, somewhere in between? We’re taking family photos because when somebody in your family is really sick, it’s a good idea to take nice family photos because you want to make sure to have those pictures and memories in case something happens. Well, technically stage IV, but staging doesn’t apply in quite the same way with choroidal melanoma that has metastasized. The short answer is that I’m doing okay, hanging in there, not sure what to think or where this is going. The long answer is four pages in a journal doesn’t describe how I’m doing. We haven’t asked about our treatment team’s success rate because this particular form of metastatic melanoma is so rare that we’ll probably be part of the success rate data set. How can you help? Be creative. Get personal. If you think of us, maybe it’s a nudge to reach out. Texts or encouraging messages work great. Yes, technically the current hardship is mostly around my husband’s illness, but there were too many bad things before this and it feels like there are a bazillion potential life implications because of this, so pretty much life feels like it’s on the line right now. And yes, I’ve heard of that. No, I haven’t heard of that. I’m not really sure what to do with any of that natural, organic, holistic stuff because the doctors told us it would be best to keep things pure so they can measure whether or not the immunotherapy treatment is working, and to not muddy the waters with alternative treatments or other things going into his body. I’m all for dietary changes because that makes total sense, but it’s all a bit overwhelming, so for now, I’m hanging on tight and trying to keep all the medical stuff managed along with every household need, child need and future-thinking need you could imagine.
(Is your head spinning? Mine is. Truth is, sometimes it’s spun so much it’s blank. Let’s just say it’s a mix between a blank brain and head spinning, somewhere in there.)
What do all these questions have in common? They’re questions of life and death. We’re facing a metastatic melanoma diagnosis, so these questions are in our face, right there, no questions barred. But if we’re completely honest with ourselves, we are ALL on our way to death. It’s just a matter of time. Will we live another day? Another week? Another month? A year? Five years? Forty five years? Who knows? Only God.
One thing this journey has taught me is that we’d all better get to living, like NOW. Today is the day the Lord has made for you, and for me. Today is the day to live, for none of us are promised one more tomorrow.
We can ask questions. We can attempt to answer. Heck, we can delay or dismiss real and hard questions about life and death. Or we can face the truth straight on. The fact that we’re able to ask questions means we’re ALIVE. We’re alive, people. So ask the questions. Ask as many as you wish. Ask away, my friend. Questions are awesome, good. But questions of life and death are often elusive. Who knows anyway. Doctors are humans. Treatment isn’t fool proof. We’re all going to die SOME day.
So live. Yes, live. Ask questions. But then live. Take family photos. Take that tropical vacation. Get a massage. Give your mama a kiss. Tell your dad you love him. Tell your friend she’s a gem. Bring a chocolate cake over to your neighbor. Do something wild and crazy. Dive deep waters. Skydive if you want to. Read that book. Write the book you can’t get out of your head. Hug your kiddos and write a secret letter they can open when they turn 21. Take the grandkids for a week. Play your trombone. Drive a convertible, ride a wild horse across the countryside. Whatever it is, do it NOW. We are not promised one more day. Today is the day to live.

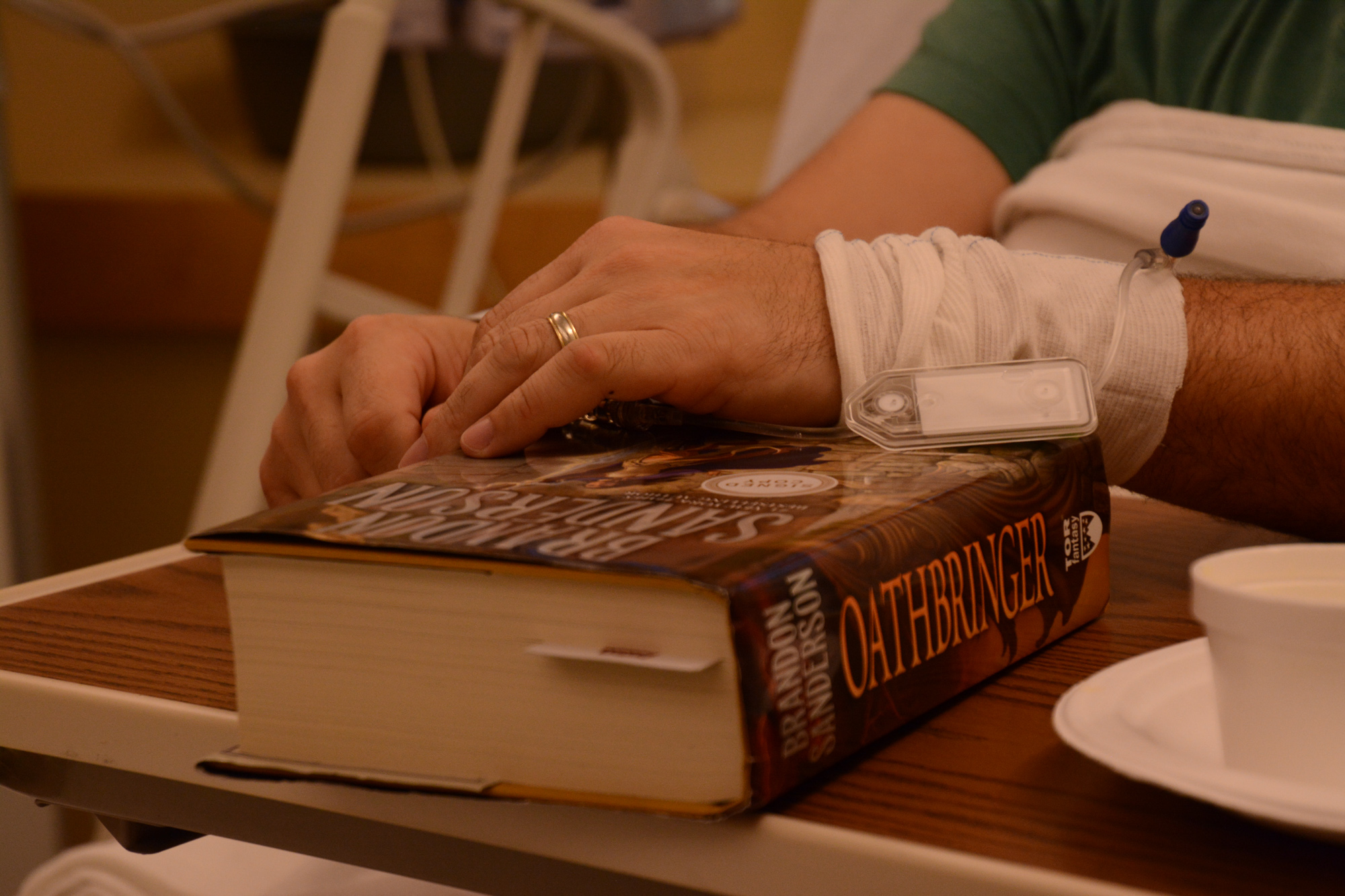
Most of you didn’t come here to read my philosophical meanderings on life, did you? I bet you have questions, like “How were Seth’s appointments today, Amy? How did treatment go? Did they give you any idea of what next steps will be?” Let me tell you, friend, then I’ll get on to the business of living. Because my husband is lying in bed next to me receiving his third infusion of immunotherapy for an incredibly rare form of metastatic melanoma. We aren’t fortune tellers. We aren’t God. We don’t know what will happen in the future. We can’t predict what our future will look like, and we can’t give anyone concrete answers about pretty much anything at this point. But we CAN decide to LIVE to the very best of our human ability. Today we will live. Today we will enjoy each other. Today we will remember to reach out and touch one another. Today we will be present, here and now. Today we will not take for granted a single second. Because TODAY is all we have.
So as for those questions y’all have. Here are some answers. These are the only answers we have for TODAY.
Labs came back perfect.
We met with a nurse who explained, once again, how immunotherapy works, all the potential side effects, and what to look out for during the course of therapy. We met with a nurse practitioner for an unusually long period of time. When you have a serious diagnosis they give you a ridiculous amount of time with doctors and nurse practitioners.
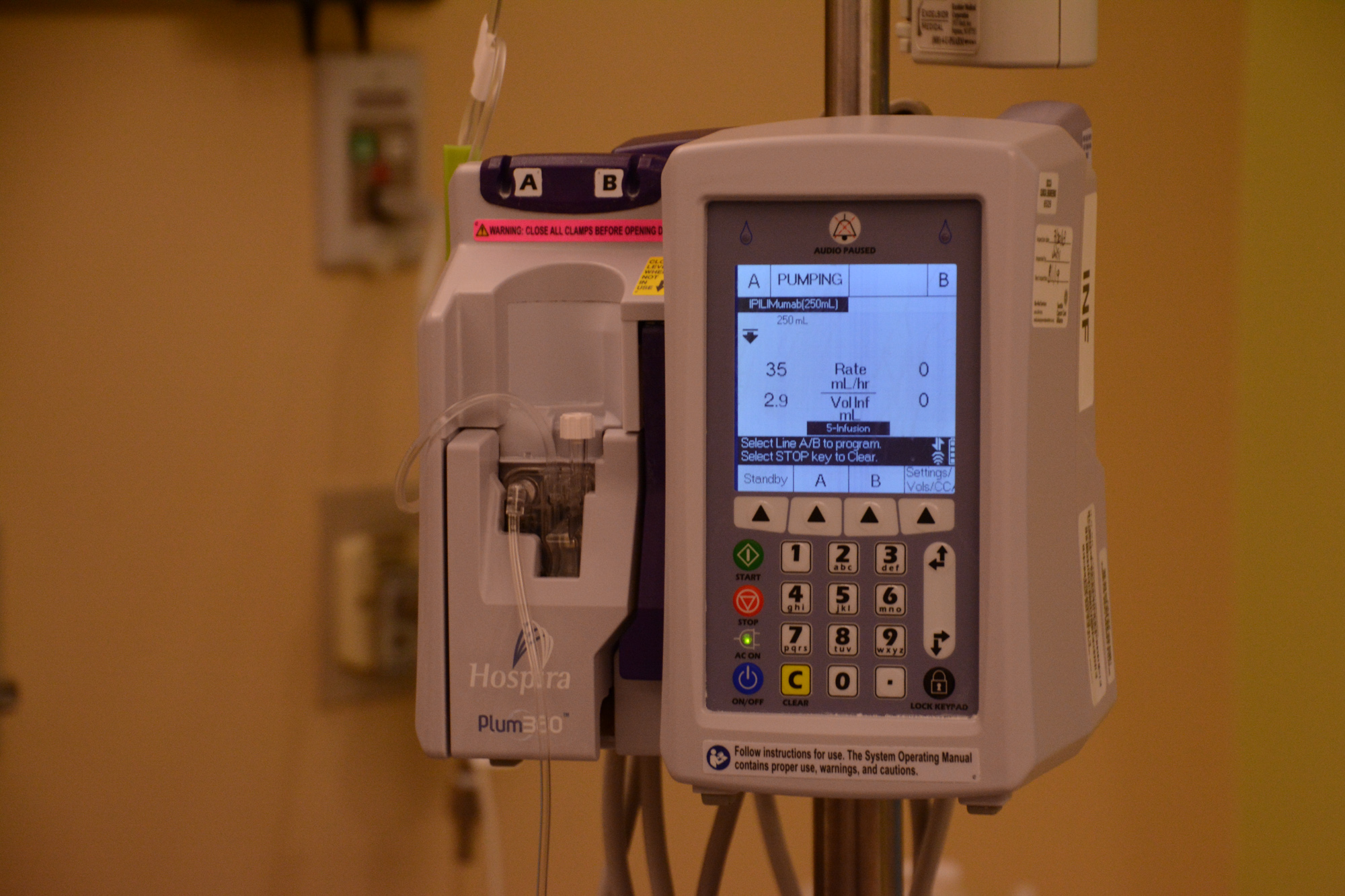
During the first two infusions of immunotherapy at Mayo Clinic, Seth received a higher dose of Yervoy and a lower dose of Opdivo. Here at Seattle Cancer Care Alliance, they dose differently. Starting today, on his third immunotherapy treatment, he is being given a lower dose of Yervoy and a higher dose of Opdivo. The goal in making this dosing change is to attempt to reduce toxicity which can cause some very serious cumulative side effects. These differences in dosing philosophies prove that even doctors don’t agree on answers. Although we are not 100% sold on the decision to change dosing, neither approach is “wrong,” so we are going with what the doctors recommend here, which is lower doses of Yervoy and higher doses of Opdivo.

Tonight, Seth is receiving his third immunotherapy treatment with infusions of both Yervoy AND Opdivo. He will receive ONE MORE Yervoy/Opdivo combo treatment three weeks from now, then after that, he will receive infusions of Opdivo only, to reduce the toxicity load that comes with combo infusions of Yervoy and Opdivo. Once he’s on the Opdivo-only treatment, there are more questions. Infuse every 2 weeks at a dose of 240 mg? Or infuse every 4 weeks at a dose of 480 mg? It will be up to the doctors and us to decide what’s best based on Seth’s unique response to treatment. More questions to come.
Another scan will happen mid-September. If the lesions stay the same or shrink, that’s good news. If they grow or spread, then treatment decisions will be made accordingly. It depends. More questions. If the growth is small (like somewhere in millimeters growth from the time it was previously measured), then they might continue with immunotherapy. If the growth is greater than millimeters and more widespread, then they would probably say immunotherapy isn’t working and try something else.
Side effects are being managed well with medication and over-the-counter meds.
We can ask questions. We can problem solve and try to fix all of life’s biggest questions around the round table (or maybe a couch if you want to get comfy). That’s good, healthy and necessary. But for some questions, there just aren’t concrete answers. For those questions, it’s better to give them a rest. Just sit. Breathe. Be. And LIVE.




















Again, Any; thanks so much for continuing to keep us in the loop! God bless and keep you held in his arms!!! Sharon Johnson